Annual Convention & Trade Show
The Annual Convention is the largest meeting of equine veterinarians in the world, anchored by more than 100 hours of continuing education; a 300-exhibitor strong trade show featuring the newest products and services for practice; and numerous social events and small discussion-oriented forums about equine veterinary medicine, as well as professional and personal development.
CE Form: If you attended the 71st Annual Convention in person and did not pick up a CE form on site, please email the AAEP at aaepoffice@aaep.org or call (859) 233-0147 to request a form.
Accessing On-Demand Convention Recordings:
The AAEP 2025 Virtual Convention platform is open and ready for you to explore!
To access it, point your browser to https://learn.aaep.org/p/AAEP2025_virtual_convention and log in using your aaep.org credentials. Your username is your email address. If you don't remember your password, use the "forgot password" link to reset it. Be sure to check out the FAQs section for tips on navigating the site.
You can earn CE from the on-demand sessions through Dec. 31, 2026.
Questions or need assistance? Please contact Karen Pautz, AAEP director of education, at kpautz@aaep.org.

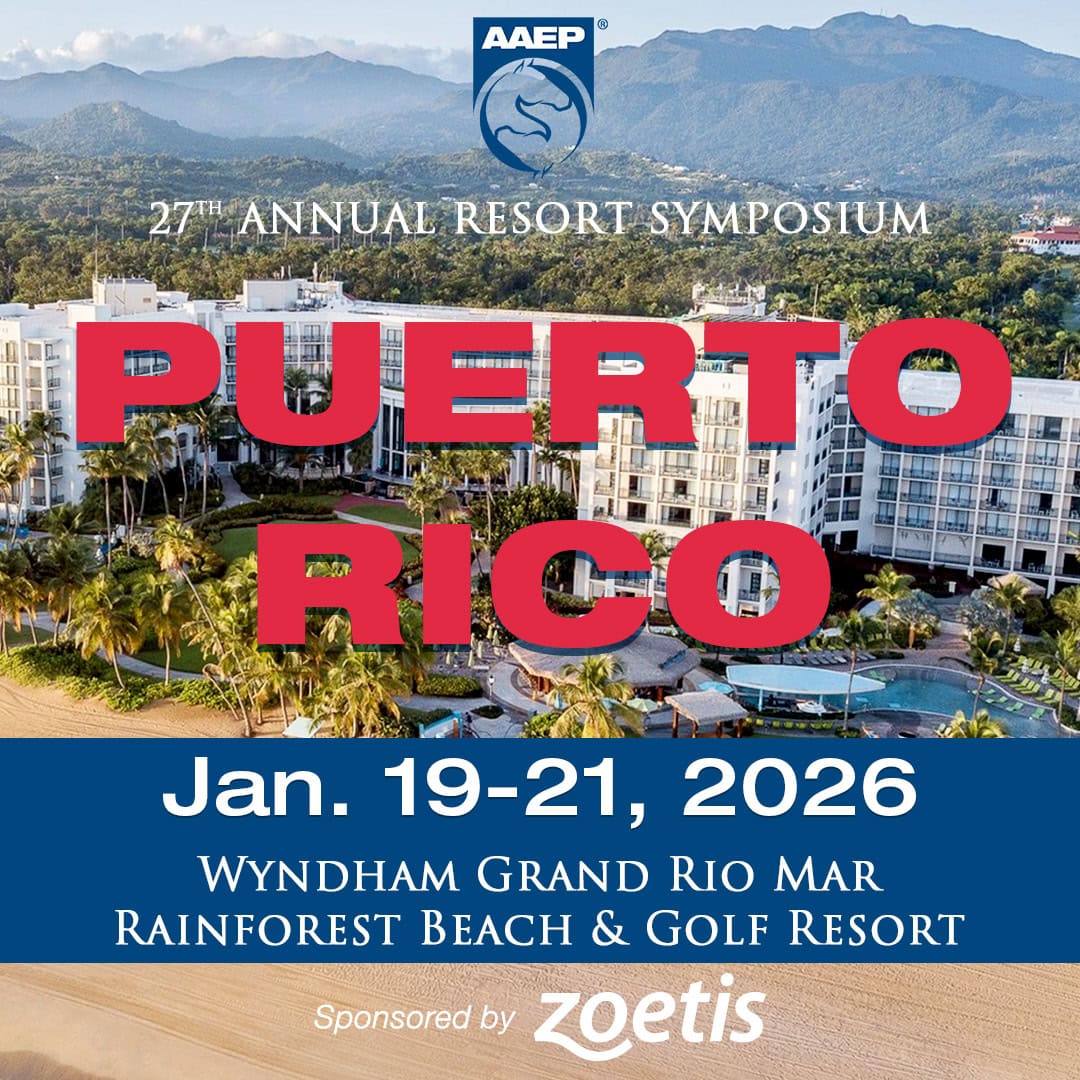
Resort Symposium
Blue skies, warm sand and turquoise waters await when the AAEP’s 27th Annual Resort Symposium heads to the luxurious Wyndham Gran Rio Mar Rainforest Beach & Golf Resort in Puerto Rico, Jan. 19–21, 2026.

Other Upcoming Events
27th Annual Resort Symposium
Saddle up for midwinter science and sun in the tropical oasis of…
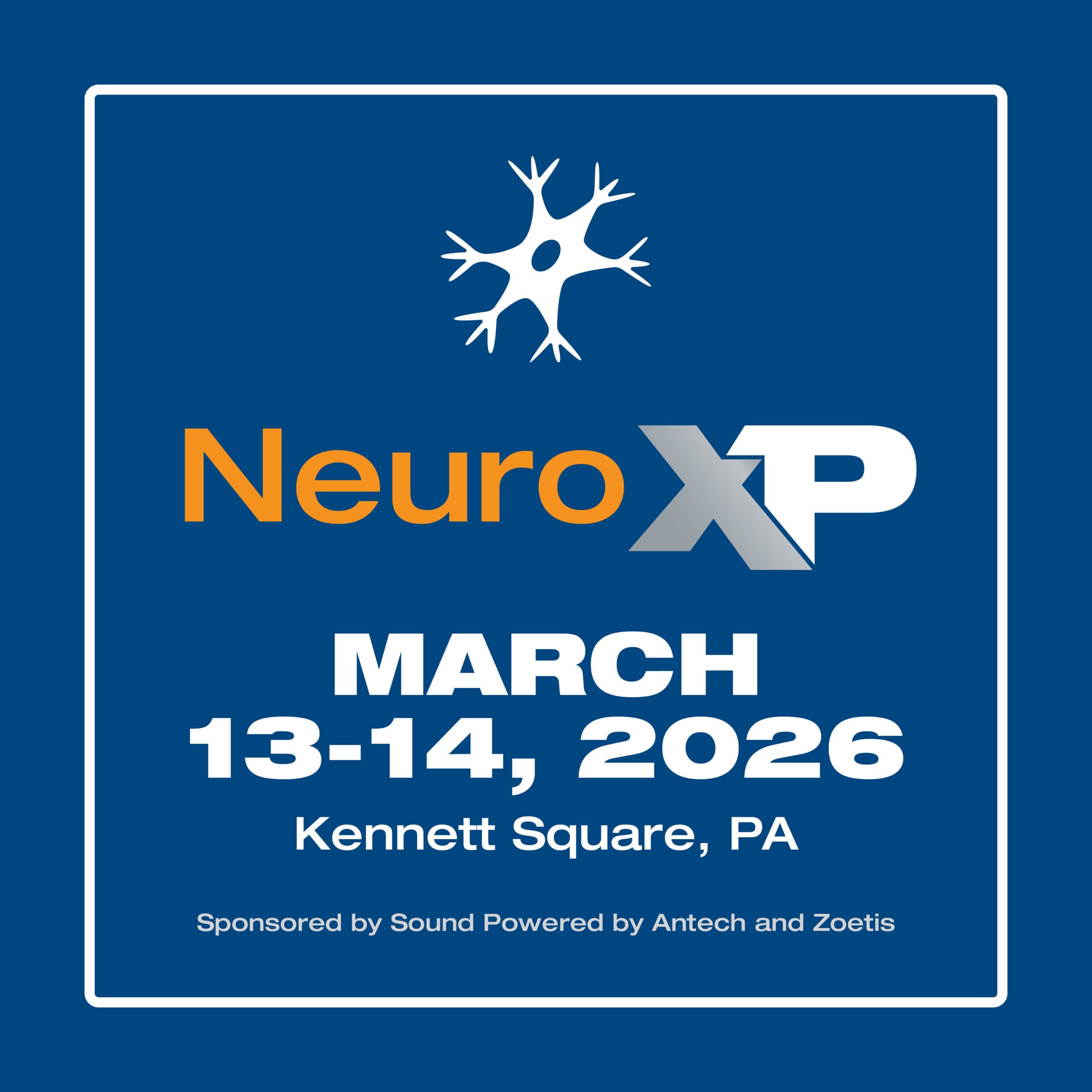
NeuroXP
Diagnosis and treatment of equine neurologic conditions is challenging, with often subtle…
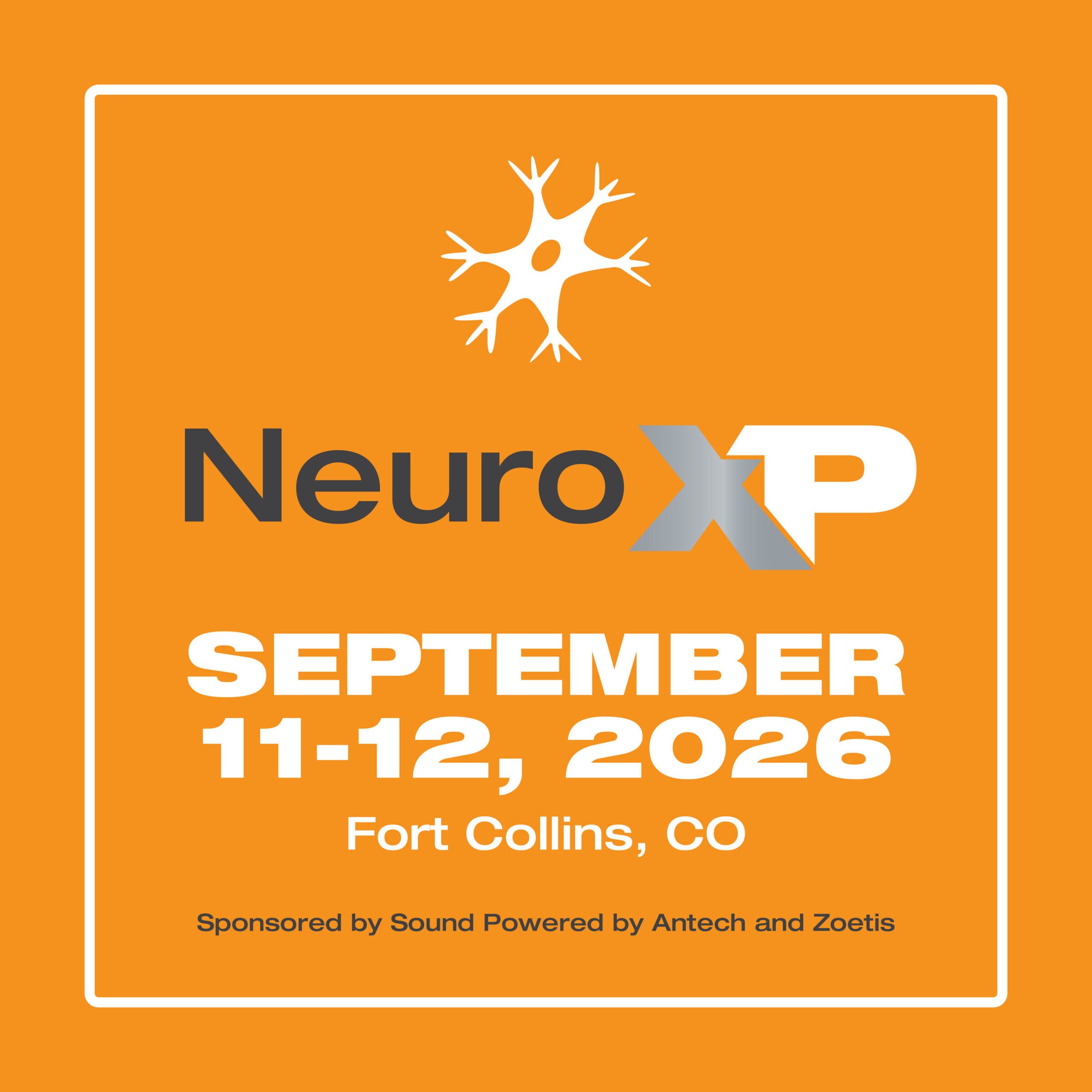
NeuroXP
Diagnosis and treatment of equine neurologic conditions is challenging, with often subtle…
More Continuing Education Opportunities
AAEP Anywhere Online CE
As a service to our members, these Continuing Education courses are available to AAEP veterinarians free of charge.
Microlearning Videos
These short, concise videos are meant to be a modern-day iteration of the classic how-to video. Use them to share procedures & recommendations with colleagues around the world.
Additional CE Opportunities
The following continuing education listings are from other, non-commercial groups or organizations outside of the AAEP.